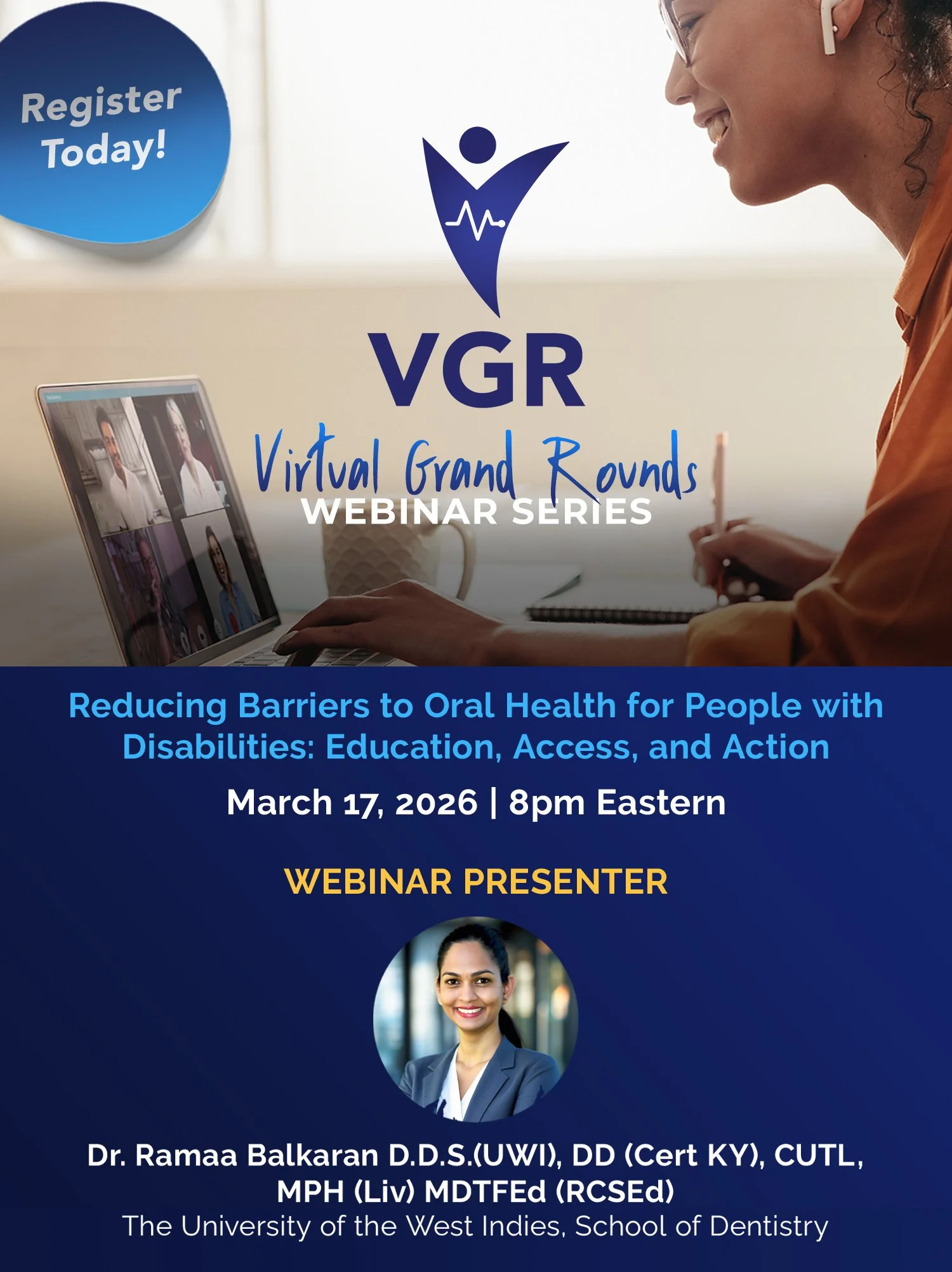
Reducing Barriers to Oral Health for People with Disabilities: Education, Access, and Action
March 17, 2026 • 8pm eastern
Dr. Ramaa Balkaran D.D.S.(UWI), DD (Cert KY), CUTL, MPH (Liv) MDTFEd (RCSEd)
This webinar examines the barriers to oral health care experienced by People with Disabilities (PWDs), including physical, financial, communication, and systemic challenges. It highlights the educational gaps that leave many Health Care Professionals underprepared to treat PWDs effectively and confidently, and highlights the lived experiences of caregivers and PWDs when accessing care.
Drawing on the perspectives of healthcare professionals, caregivers, and self-advocates, the session presents practical, evidence-informed solutions to promote more accessible, inclusive, and equitable oral health systems.
Dr. Balkaran is a part-time Lecturer in Special Needs Dentistry at the University of the West Indies and a part-time Research Assistant at the University of Toronto. She completed postgraduate clinical training in International Developmental Dentistry at the University of Louisville School of Dentistry in Kentucky, USA, and holds a Master of Public Health with a Specialisation in Management of Health Systems from the University of Liverpool. Dr. Balkaran is currently awaiting the defense of her PhD at the University of Turku, where her research evaluates oral health care for people with disabilities.
She currently serves as a Board Member of the Canadian Society of Oral Health and Disability, where she chairs the Research and Education Committee, and is also a member of the Network for Canadian Oral Health Research (NCOHR). From 2022 to 2024, she served as Vice President of the International Association for Dental Research Caribbean Section.
Dr. Balkaran has actively participated in community dental outreach initiatives and has successfully secured funding for treatment and equipment to improve access to care for individuals with disabilities. She has authored twenty-eight peer-reviewed publications. Her research focuses on the intersection of general health and oral diseases, with particular emphasis on oral health promotion and disease prevention, especially among medically compromised individuals and those with special needs.
Every THIRD Tuesday* of the month the AADMD Student & Resident Committee hosts interdisciplinary webinars for clinicians to learn from colleagues in a patient-centered manner with the purpose of encouraging comprehensive care provision to patients with IDD.
*Day of the week is subject to change.
PAST WEBINARS
2019-2025
All webinars are available to re-watch through AADMD’s One Voice Network.
Students/Residents always watch for free, others must have a paid subscription, starting at just $50 a year.